Antibiotic resistance is a growing concern in the field of medicine and public health. It occurs when bacteria evolve mechanisms to resist the effects of drugs that once effectively treated infections. This phenomenon can lead to prolonged illness, increased healthcare costs, and a greater risk of disease spread.
Understanding how bacteria become resistant to antibiotics is crucial for developing strategies to combat this public health crisis.
Mechanisms of Resistance
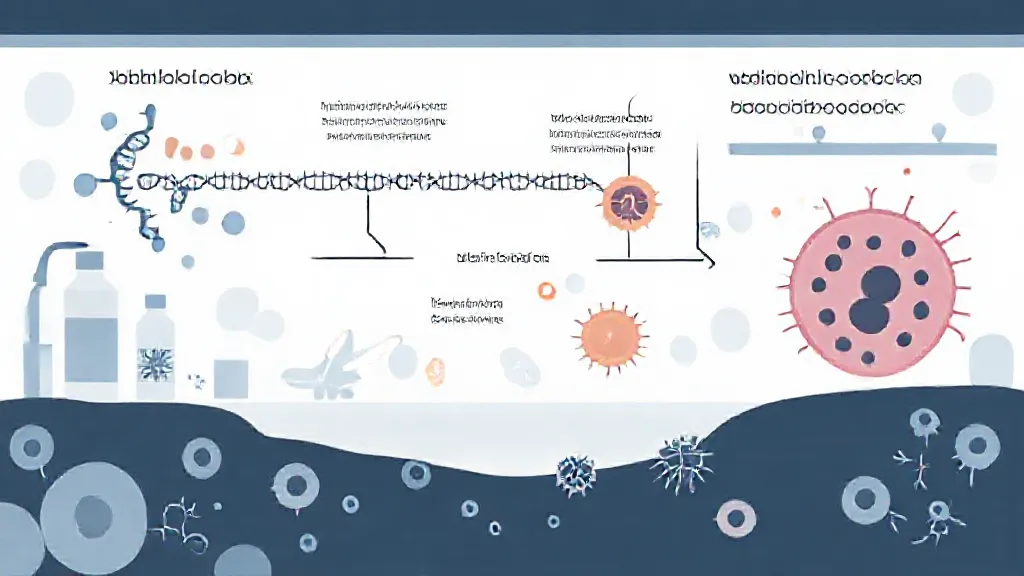
Bacteria can become resistant to antibiotics through several mechanisms. One of the most common is genetic mutation.
Bacteria reproduce rapidly, and during this process, random mutations can occur in their DNA. Some of these mutations may provide a survival advantage in the presence of an antibiotic. For example, a mutation might alter the bacterial cell wall, preventing the antibiotic from entering.
Another mechanism is horizontal gene transfer, where bacteria can acquire resistance genes from other bacteria through processes such as transformation, transduction, or conjugation. This allows for rapid dissemination of resistance traits among bacterial populations.
The Role of Antibiotic Overuse
The overuse and misuse of antibiotics in both human medicine and agriculture significantly contribute to the development of antibiotic resistance.
When antibiotics are prescribed unnecessarily or when patients do not complete their prescribed course, it creates an environment where only the strongest bacteria survive. In agriculture, the use of antibiotics for growth promotion in livestock can also lead to resistant strains of bacteria that can be transferred to humans through the food chain.
Historical Context of Antibiotic Resistance
The history of antibiotic resistance dates back to the discovery of penicillin in the 1920s.
Initially hailed as a miracle drug, penicillin's effectiveness against bacterial infections was soon challenged by the emergence of resistant strains. By the 1940s, penicillin-resistant Staphylococcus aureus was already identified. This historical context highlights the ongoing battle between antibiotic development and bacterial adaptation, underscoring the need for continual research and monitoring.
Impact on Public Health
The rise of antibiotic-resistant bacteria poses a significant threat to public health. Infections caused by resistant bacteria can lead to longer hospital stays, higher medical costs, and increased mortality. The World Health Organization has declared antibiotic resistance one of the top ten global public health threats facing humanity.
Infections such as methicillin-resistant Staphylococcus aureus (MRSA) and multidrug-resistant tuberculosis (MDR-TB) exemplify the severe consequences of this issue.
Preventative Measures
To combat antibiotic resistance, several strategies can be implemented. Promoting the responsible use of antibiotics is essential.
This includes prescribing antibiotics only when necessary and ensuring patients complete their treatment courses. Additionally, improving infection prevention and control measures in healthcare settings can help reduce the spread of resistant bacteria. Public education campaigns can also raise awareness about the importance of antibiotic stewardship.
The Future of Antibiotic Development
Researchers are exploring new avenues for antibiotic development to stay ahead of resistant bacteria. This includes the discovery of novel antibiotics, the development of bacteriophage therapy, and the use of combination therapies that enhance the effectiveness of existing antibiotics. Furthermore, advancements in genetic engineering and synthetic biology may offer new strategies for combating resistance.
Conclusion: A Collaborative Approach
Addressing antibiotic resistance requires a collaborative approach involving healthcare professionals, policymakers, researchers, and the public. By understanding the mechanisms behind bacterial resistance and taking proactive measures, we can work towards preserving the efficacy of antibiotics for future generations. Ongoing research, education, and responsible antibiotic use are essential components in the fight against this pressing global health challenge.