Chronic pain is a complex and multifaceted condition that affects millions of people worldwide. Unlike acute pain, which serves as a warning signal for injury or illness, chronic pain persists for months or even years, often without a clear cause. Understanding where chronic pain stems from in the body requires an exploration of its biological, psychological, and social dimensions.
The Biological Basis of Chronic Pain
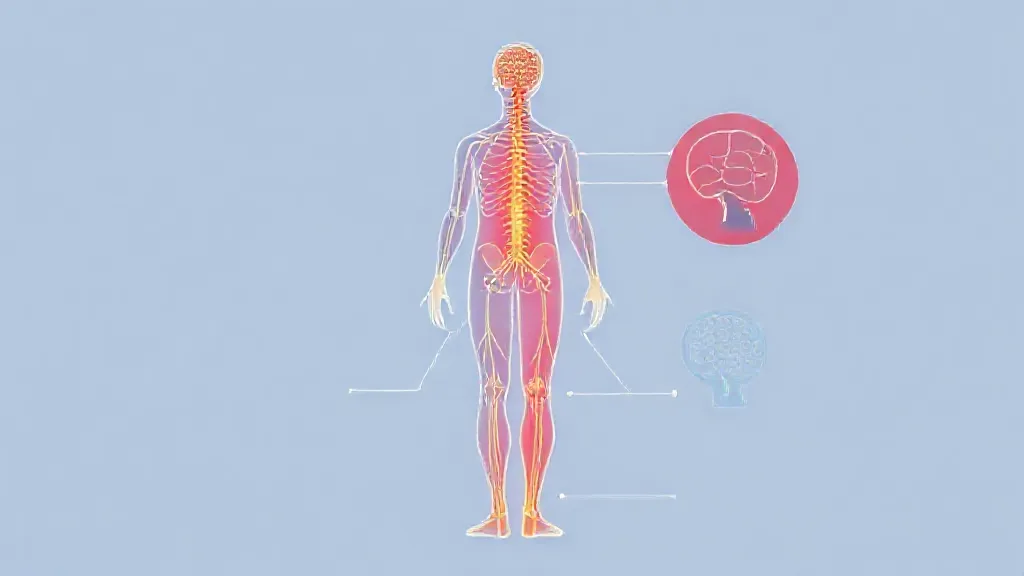
Chronic pain often arises from changes in the nervous system. When tissue damage occurs, the body’s nociceptors—specialized nerve endings—send pain signals to the brain. In cases of chronic pain, these signals may become dysregulated, leading to a condition known as central sensitization.
This phenomenon occurs when the nervous system becomes hyper-responsive to stimuli, causing even non-painful stimuli to be perceived as painful. Research has shown that conditions such as fibromyalgia and chronic fatigue syndrome are associated with this heightened sensitivity.
Psychological Factors and Chronic Pain
The experience of chronic pain is not solely a physical phenomenon; psychological factors play a significant role.
Anxiety, depression, and stress can exacerbate the perception of pain. Studies indicate that individuals with a history of trauma or psychological distress may be more susceptible to developing chronic pain conditions. Cognitive-behavioral therapy (CBT) has emerged as an effective treatment strategy, helping individuals manage their pain by addressing negative thought patterns and emotional responses.
Inflammation and Chronic Pain
Inflammation is another critical factor in the development of chronic pain. Conditions such as arthritis, which involve persistent inflammation of the joints, can lead to long-lasting pain. Inflammatory mediators, such as cytokines and prostaglandins, can sensitize nociceptors and prolong the pain experience.
Moreover, chronic inflammation can alter pain pathways in the nervous system, further contributing to the persistence of pain.
Neuropathic Pain: A Unique Challenge
Neuropathic pain, which arises from damage to the nervous system itself, presents a unique challenge in understanding chronic pain. Conditions such as diabetic neuropathy, post-herpetic neuralgia, and multiple sclerosis can lead to neuropathic pain, characterized by sensations of burning, tingling, or shooting pain.
This type of pain often requires different treatment approaches, including medications like anticonvulsants or antidepressants that target nerve pain specifically.
The Role of Lifestyle Factors
Lifestyle factors, including diet, exercise, and sleep, can significantly influence chronic pain. Poor nutrition can lead to obesity, which places additional strain on joints and exacerbates conditions like osteoarthritis.
Lack of physical activity can weaken muscles and lead to further pain. Conversely, regular exercise has been shown to improve pain management and enhance overall well-being. Sleep disturbances, common in individuals with chronic pain, can also create a vicious cycle, as inadequate rest can heighten pain sensitivity.
The Impact of Social Determinants
Social determinants of health, such as socioeconomic status, access to healthcare, and social support networks, play a crucial role in the experience of chronic pain. Individuals from lower socioeconomic backgrounds may face barriers to receiving adequate medical care, leading to untreated or poorly managed pain. Additionally, social isolation can exacerbate feelings of depression and anxiety, further complicating the pain experience.
Integrative Approaches to Pain Management
Given the multifaceted nature of chronic pain, integrative approaches that combine medical, psychological, and lifestyle interventions are essential. Pain management programs often include physical therapy, medication management, psychological support, and lifestyle modifications. Complementary therapies, such as acupuncture, massage, and mindfulness practices, have also gained popularity as adjuncts to traditional pain management strategies.
Conclusion: The Future of Chronic Pain Research
Understanding where chronic pain stems from in the body is an ongoing area of research. Advances in neuroscience, psychology, and pain management are continually shaping our understanding of this complex condition. As we learn more about the biological, psychological, and social factors that contribute to chronic pain, we can develop more effective treatment strategies and improve the quality of life for those affected.