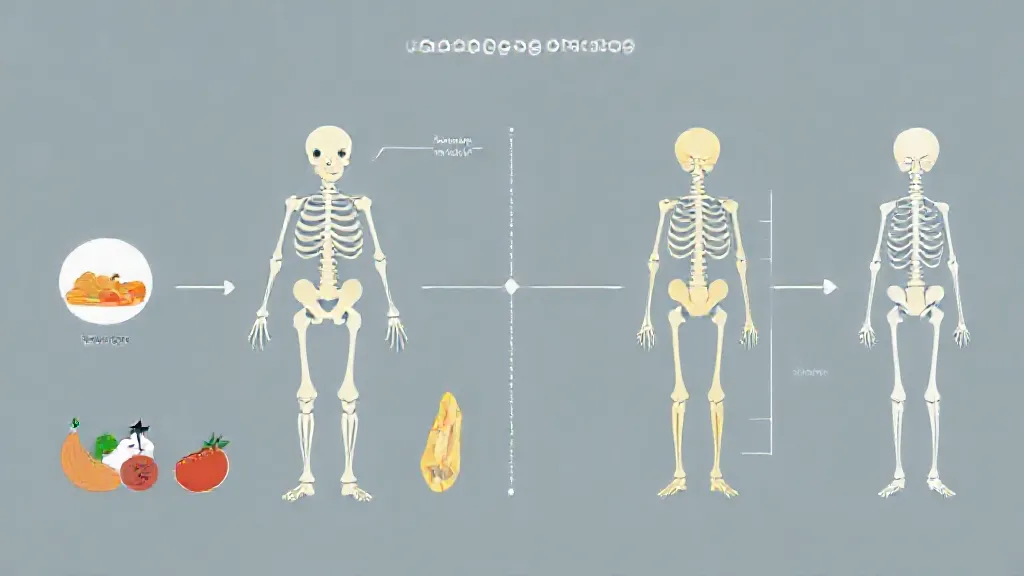
Aging is a natural process that affects every aspect of human biology, including bone strength. As individuals age, they experience a gradual decline in bone density and strength, leading to an increased risk of fractures and osteoporosis. Understanding how aging impacts bone health is crucial for developing preventive strategies and promoting overall well-being in older adults.
The Biological Mechanisms of Bone Aging
Bone is a dynamic tissue that undergoes continuous remodeling, a process involving the resorption of old bone and the formation of new bone. This balance is maintained by osteoblasts (bone-forming cells) and osteoclasts (bone-resorbing cells). As people age, the activity of osteoblasts decreases while osteoclast activity remains relatively constant or may even increase.
This imbalance leads to a net loss of bone mass, particularly in trabecular bone, which is found in the spine and ends of long bones. Studies have shown that after the age of 30, bone mass begins to decline at a rate of about 0.5% to 1% per year, accelerating in women post-menopause due to hormonal changes.
The Role of Hormones in Bone Health
Hormones play a significant role in regulating bone density. Estrogen, for instance, is vital for maintaining bone mass in women. The decline in estrogen levels during menopause leads to an increase in bone resorption, contributing to the rapid loss of bone density observed in postmenopausal women.
Similarly, testosterone levels in men decrease with age, which can also affect bone density. Research indicates that men with lower testosterone levels are at a higher risk for osteoporosis and fractures. Understanding the hormonal changes associated with aging is essential for developing targeted treatments to preserve bone health.
Nutritional Factors Influencing Bone Strength
Nutrition is a critical factor in maintaining bone health throughout life. Calcium and vitamin D are particularly important for bone strength. Calcium is a key component of bone tissue, while vitamin D facilitates calcium absorption in the body.
As individuals age, dietary intake of these nutrients often declines, exacerbating the risk of osteoporosis. The recommended dietary allowance for calcium is 1,200 mg per day for older adults, and for vitamin D, it is 800 to 1,000 IU. Ensuring adequate nutrition is vital for supporting bone health and preventing age-related bone loss.
Physical Activity and Bone Density
Regular physical activity is known to have a positive impact on bone health. Weight-bearing exercises, such as walking, jogging, and resistance training, stimulate bone formation and help maintain or even increase bone density. Studies show that older adults who engage in consistent physical activity have a lower risk of fractures and osteoporosis.
Conversely, sedentary lifestyles can lead to accelerated bone loss. Incorporating exercise into daily routines is essential for promoting bone strength and overall health in aging populations.
The Impact of Lifestyle Choices on Bone Health
Lifestyle choices, including smoking and alcohol consumption, can significantly affect bone strength.
Smoking has been linked to decreased bone density and an increased risk of fractures due to its negative impact on bone remodeling. Alcohol, when consumed excessively, can interfere with calcium absorption and hormone levels, further compromising bone health. Encouraging healthy lifestyle choices is crucial for mitigating the effects of aging on bone strength and reducing the risk of osteoporosis.
The Importance of Early Intervention
Early intervention is key to preventing age-related bone loss. Regular bone density screenings can help detect osteoporosis before fractures occur. Additionally, lifestyle modifications, nutritional supplementation, and pharmacological treatments can be implemented to support bone health.
For example, bisphosphonates are commonly prescribed to help strengthen bones in individuals diagnosed with osteoporosis. Education about the importance of bone health should begin early in life, emphasizing the need for preventive measures as individuals age.
Future Research Directions in Bone Health
Ongoing research is critical for understanding the complex mechanisms behind aging and bone strength.
Scientists are exploring new therapeutic approaches, including biologics and gene therapies, that may offer innovative ways to enhance bone regeneration and repair. Furthermore, studies are investigating the role of gut microbiota in bone health, as emerging evidence suggests that the gut-brain-bone axis may influence bone metabolism. Continued research will provide valuable insights into preventing and treating age-related bone loss.
Conclusion: Promoting Healthy Bones in Aging
In conclusion, aging has a profound impact on bone strength due to a combination of biological, hormonal, nutritional, and lifestyle factors. By understanding these influences, individuals can take proactive steps to maintain bone health as they age. Emphasizing the importance of nutrition, physical activity, and healthy lifestyle choices, along with early intervention and ongoing research, will be essential for promoting strong bones and reducing the risk of osteoporosis in older adults.